Not long ago, I found myself totally baffled when my mom called to say she couldn’t remember where she put her car keys or why she’d wandered into a room. Sure, everyone jokes about brain fog, but it wasn’t until I stumbled upon Dr. Lisa Mosconi’s work that I realized menopause could be the root cause—and not just for my mom, but for millions. This blog dives into what happens to the brain during menopause, the real science beneath the stereotypes, and why everyone—yes, even men—should pay attention. Spoiler: it’s not all doom and gloom. In fact, embracing the brain’s midlife makeover might just change how we see ourselves and each other.
From Hot Flashes to Brain Fog: Unpacking the Sensational Symptoms
If you’ve ever wondered why menopause symptoms like hot flashes, brain fog, night sweats, insomnia, and memory lapses seem to take over your life, you’re not alone. These aren’t just passing discomforts—they’re part of a profound neurological shift happening in your brain. For years, women have described these sensations, and now, research is finally catching up to what you’ve been saying all along.
"This is evidence of what women have been saying all along: menopause changes the functionality of your brain." (0:00-0:02)
Let’s start with the basics. As menopause approaches, you might notice that brain fog—that frustrating sense of mental cloudiness—often arrives alongside insomnia and night sweats. It’s not just you: studies reveal that roughly two-thirds of women experience cognitive symptoms like these during menopause (0:46-0:49). These aren’t simply hormonal quirks. Instead, they’re rooted in real, measurable changes in your brain’s chemistry and function.
Groundbreaking research by Dr. Lisa Mosconi, a leading neuroscientist, has revolutionized our understanding of menopause’s impact on the brain (0:18-0:24). Using advanced brain imaging, Dr. Mosconi’s team discovered that during menopause, the brain’s energy levels can drop by a staggering 30% (0:39-0:42). Imagine your brain running on a third less fuel—no wonder symptoms like memory lapses, depression, and anxiety become more common.
What’s happening under the surface? As estrogen levels decline, your brain undergoes significant changes, including alterations in estrogen receptors. This shift doesn’t just affect mood or sleep—it can fundamentally alter how your brain works, leading to the classic menopause symptoms that so many women report. Yet, surprisingly, traditional stereotypes about menopause often ignore these neurological symptoms, focusing instead on the physical or emotional aspects.
"Two-thirds of all women experience brain fog—those are brain symptoms not recognized in medicine." (0:49-0:52)
It’s also important to recognize that not all women experience menopause symptoms the same way. Research shows that Black and Hispanic women often face more severe symptoms than their white counterparts (0:54-0:57). This health disparity highlights the need for more inclusive research and better support for all women navigating menopause.
Historically, the medical field has sometimes dismissed these symptoms, labeling women as “mentally unstable” rather than acknowledging the neurological roots of their experiences. But now, with evidence from brain imaging and large-scale studies, it’s clear that menopause symptoms like hot flashes, insomnia, memory lapses, depression, and anxiety are deeply connected to changes in brain function.
So, when you notice your mind feeling foggy or your sleep disrupted, remember: these are real, brain-based symptoms. Understanding this can help you—and your healthcare provider—navigate the menopausal journey with more clarity and compassion.
Meet the Brain Detective: Dr. Lisa Mosconi and the Science Revolution
If you’ve ever wondered how menopause truly affects your mind, you’re not alone. Dr. Lisa Mosconi, a leading figure in neuroscience research, has made it her mission to answer this question using the latest in brain imaging technology. Her journey into the world of women’s health began with a single, unforgettable moment: witnessing the neurological toll of hot flashes on a study participant. That “aha moment” set her on a path that would change how we understand menopause’s impact on the brain (0.18–0.27).
Dr. Mosconi holds a PhD in neuroscience and nuclear medicine, specializing in brain imaging—a field where science meets the inner workings of the mind (6.33–6.41). As director of the Women’s Brain Initiative at New York Presbyterian and Weill Cornell, she leads a team at the very forefront of reproductive neuroscience. Or, as she puts it,
“Our team is at the Forefront of reproductive neuroscience or gender neurology.”(7.10–7.14)
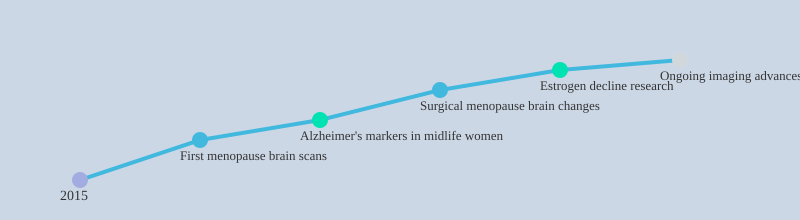
What sets Dr. Mosconi’s work apart is her focus on the brain’s midlife transformation. She and her team were the first to conduct brain scans comparing women before and after menopause, as well as after surgical menopause (removal of the ovaries). These studies revealed something striking: the brains of menopausal women show early signs of Alzheimer’s—plaques and other “red flags”—years before men of the same age do (7.49–8.04). In fact, nearly two-thirds of Alzheimer’s patients are women, and the risk rises sharply after menopause. This is not just a coincidence; research shows that declining estrogen levels during menopause play a key role in these changes.
Over the past decade, Dr. Mosconi has published more than 150 scientific papers, mapping how the female brain changes during pre-, peri-, and post-menopause. Her lab’s advanced brain imaging techniques allow researchers to see, in real time, how estrogen decline affects brain structure and function. The findings are clear: menopause is not just a reproductive transition—it’s a neurological one, too.
Surgical menopause, which involves removing the ovaries, offers even more insight. Brain scans of women who have undergone this procedure show distinctive changes, deepening our understanding of estrogen’s protective role in brain health. These discoveries are helping to explain why women are more vulnerable to neurodegenerative diseases like Alzheimer’s, especially after midlife.
For Dr. Mosconi, this research is also personal. With a family history of Alzheimer’s, her drive to solve the puzzle of women’s brain health is both professional and deeply heartfelt. Her work is not just about science—it’s about giving women the knowledge and tools to thrive during one of life’s biggest transitions.
“You did the first brain scans on a woman’s brain to compare before and after menopause.”
Dr. Lisa Mosconi’s neuroscience research is revolutionizing our understanding of menopause’s impact on women’s health. With every new discovery, she brings us closer to unlocking the secrets of the female brain—and to a future where women can navigate midlife with confidence and clarity.
Tracking the Turmoil: Symptom Diaries, Menopause Scales, and Personal Data
If you’ve ever wondered how to make sense of the chaos that menopause brings to your mind and body, you’re not alone. Many women, even those who’ve had open conversations about menopause (see transcript 4.08–4.25), are surprised to learn that so many symptoms—like brain fog, insomnia, and mood swings—are actually neurological. These symptoms aren’t just about your ovaries; they’re rooted in the brain (6.09–6.22). That’s why tracking what you’re experiencing can be so powerful.
Symptom monitoring is more than just jotting down how you feel. Tools like the Menopause Rating Scale, Hot Flush Scale, and a simple Symptom Diary help you and your healthcare provider quantify what’s happening. These tools might not be perfect, but they’re empowering. They give structure to what often feels like a messy, unpredictable experience.
Why Track Symptoms? The Real-World Value
Keeping a symptom diary doesn’t just help you remember what happened last week. It can reveal patterns: maybe your brain fog is worse after a poor night’s sleep, or hot flushes spike after a stressful day. This kind of personal data capture can help you spot triggers and make small adjustments that have a real impact on your daily life.
Doctors are increasingly recommending these tools, not just for research but for everyday use. As Dr. Lisa Mosconi, a leading neuroscientist, points out, understanding the brain’s role in menopause is crucial for effective symptom management (6.24–6.59). And research shows that when you track your symptoms, you’re more likely to find ways to manage them.
Validated Tools: From Clinical Trials to Your Daily Routine
The Menopause Rating Scale and Hot Flush Scale are validated questionnaires used in both clinical trials and real-world settings. They help measure the frequency and severity of symptoms, providing a common language for women and healthcare professionals. This is especially important in clinical research, where consistency is key.
But it’s not just about numbers. Studies—including randomized controlled trials and meta-analyses—show that using symptom diaries can actually reduce hot flush frequency by up to 50%. Meta-analyses confirm that personal monitoring shortens the duration of symptoms and improves quality of life. In other words, tracking works.
"Symptom monitoring tools and diaries can help women and healthcare providers track and manage menopausal symptoms more effectively."
How Symptom Monitoring Tools Compare
| Tool | Key Benefit | Research Backing |
|---|---|---|
| Symptom Diary | Reduces hot flush frequency by up to 50% | RCTs |
| Menopause Rating Scale | Tracks symptom burden in clinics and research | Widely used, validated |
| Hot Flush Scale | Measures severity and frequency of hot flushes | Meta-analyses confirm improved outcomes |
So, if you’re navigating menopause, consider making symptom monitoring part of your toolkit. It’s a simple step that can bring clarity, support conversations with your doctor, and—according to research—help you feel better, faster.
Behind the Scenes: What Actually Happens in the Menopausal Brain?
When you think about menopause, you probably picture the end of periods and fertility. But there’s a lot more going on beneath the surface—especially in your brain. In fact, research shows that menopause is less like a simple “off switch” for reproduction and more like an extreme home makeover for your mind (4:56–5:26). Let’s pull back the curtain and see what’s really happening in the menopausal brain.
Menopause: The Brain’s Extreme Makeover
Most people know that menopause means the end of menstrual cycles, usually around midlife (5:09–5:16). What’s less obvious is that this transition triggers profound brain changes. Dr. Lisa Mosconi, a leading researcher in women’s brain health, describes menopause as a “renovation project on the brain”—not just a loss, but a major reorganization (5:26–5:29). She emphasizes that estrogen decline isn’t just a footnote; it actually sets off a cascade of changes in your brain’s chemistry and structure.
Estrogen Decline: More Than Just Hormones
Estrogen is well known for its role in reproduction, but it’s also a key player in cognitive effects and brain health. As estrogen levels drop during menopause, your brain’s neurochemistry and even its physical structure start to shift. Advanced brain imaging studies confirm that this isn’t just theoretical—these changes are visible and measurable. For example, Mosconi’s research shows that estrogen decline during menopause triggers both functional and anatomical brain changes, which can impact memory, attention, and mood (5:26–5:37).
Brain Imaging Reveals Early Alzheimer’s Indicators
One of the most striking findings from recent studies is the difference in Alzheimer’s risk between women and men. Brain scans reveal a significant increase in Alzheimer’s plaques in perimenopausal women compared to men of the same age (10:29–11:14). These red flags appear much earlier in women’s brains, often during the menopause stages—long before any symptoms of memory loss or cognitive decline become obvious. This suggests that the menopause transition is a critical window for brain health interventions.
| Finding | Details |
|---|---|
| Alzheimer’s Plaques | Increased in perimenopausal women vs. men (statistically significant, per Mosconi’s research) |
| Estrogen Decline Effects | Triggers functional and anatomical brain changes (confirmed by imaging) |
| Menopause Timing | Typically occurs in midlife (age range implied) |
Estrogen Receptors: The Brain’s Secret Strength?
Even after menopause, estrogen receptors remain active in the brain. This could be a clue to why some women remain resilient, while others face greater risk for cognitive decline. Researchers are now exploring how these receptors might help protect the brain or, conversely, contribute to vulnerability if estrogen support is lost.
“Menopause is actually a renovation project on the brain.”
So, while menopause marks the end of fertility, it’s also a time of major brain changes—a neurological transformation that’s only beginning to be understood. With new brain imaging technologies and ongoing research, we’re finally starting to see the full picture of what menopause really means for women’s minds.
Kitchen Miracles & Couch Science: Real-Life Tweaks That Boost Brain Health
When it comes to menopause, your brain is right at the center of the action. Many of the most common menopause symptoms—like hot flashes, memory lapses, mood swings, and sleep issues—actually start in the brain. But here’s some good news: research shows that simple lifestyle adjustments can make a real difference in how you feel and how your brain functions during this major life transition (1.09-1.11).
The Mediterranean Diet: Food as Medicine
Let’s start in the kitchen. You might have heard the buzz about the Mediterranean Diet, and for good reason. Studies indicate that this way of eating—rich in vegetables, fruits, whole grains, nuts, olive oil, and fish—does more than just support your heart. It may actually delay the onset of menopause by up to three years (1.21-1.27). As one expert put it:
"A diet rich in [Mediterranean foods] has been linked with a later onset of menopause by 3 years."
That’s right—what’s on your plate could be influencing when menopause starts, and how your brain weathers the changes. This isn’t just about delaying symptoms, but also about supporting long-term brain health. Research is increasingly showing that dietary patterns like the Mediterranean Diet can help reduce cognitive effects and lower the risk of neurodegenerative diseases, such as Alzheimer’s (10.54-11.23).
Exercise Impact: Move for Your Mind
It’s not all about food. Exercise is another pillar of brain health during menopause. Routine physical activity—whether it’s brisk walking, yoga, or dancing in your living room—has been shown to support memory, mood, and overall brain energy. Even moderate movement can help manage menopause symptoms and reduce cognitive decline. You don’t need to run marathons; small, consistent efforts add up over time.
Stacking Up Small Wins
Here’s the thing: brain-healthy living isn’t about perfection. It’s about stacking up small wins. Maybe you swapped out a sugary snack for a handful of nuts. Or you took the stairs instead of the elevator. Each choice, no matter how minor it seems, contributes to your overall brain health and helps manage menopause symptoms. Over time, these little victories—like fewer “where-are-my-keys?” moments—are worth celebrating.
Tracking Progress and Building Resilience
Don’t expect instant results. Lifestyle adjustments often work gradually, and symptom improvement can be subtle at first. That’s why tracking your progress—whether with a journal, an app, or a simple calendar—can be so helpful. Not only does it help you notice patterns, but it also builds optimism and resilience. Seeing even small improvements can boost your motivation to keep going.
Lifestyle Adjustments: Your Brain’s Secret Weapon
Emerging evidence suggests that lifestyle changes may serve as another line of defense against Alzheimer’s and other cognitive effects of menopause. In fact, some studies show that these adjustments can matter as much as genetics or hormones when it comes to brain health. So, while menopause can feel overwhelming, remember: you have real, concrete ways to support your mind and body—starting right in your own kitchen and living room.
Why Men, Families, and the World Should Care About the ‘Women’s Brain Issue’
When you hear the phrase “menopause impact,” it’s easy to think it’s just a women’s health concern. But if you look closer, you’ll see that menopause is not a solitary journey. It’s a transition that touches families, friendships, and even the fabric of society (2.18-2.22). Understanding what happens in a woman’s brain during menopause isn’t just for women—it’s for everyone who cares about family support, healthy relationships, and the wellbeing of those around them.
Why should you, as a man, son, partner, or friend, care about the cognitive effects of menopause? The answer is simple: women are important, and their health matters. For too long, women’s health has been overlooked in both society and medicine (2.37-2.45). Now, research shows that supporting women through menopause leads to stronger families and healthier communities. When you understand what your spouse, mother, sister, or daughter is experiencing, you’re better equipped to offer empathy and practical support (2.32-2.41).
Dr. Lisa Mosconi, a leading voice in menopause research, often receives heartfelt messages from men who say, “You really helped me understand my wife better… Now as a family we’re making different decisions or we’re having different conversations.” These stories highlight a powerful truth: when men learn about menopause, they help break down old stereotypes and build bridges of understanding within their families (2.24-2.41).
- Menopause isn’t just a ‘women’s issue’. It affects household dynamics, healthcare decisions, and the emotional climate at home.
- Family support is vital. Studies indicate that when families are informed and supportive, women experience less stress and better health outcomes during the menopausal transition.
- Healthcare provider education matters. When doctors and nurses understand menopause’s cognitive effects, they can offer better care and guidance for the whole family.
Consider this: almost two-thirds of Alzheimer’s patients are women. That statistic alone shows how menopause and brain health are deeply connected—not just for individuals, but for countless families facing the challenges of aging and memory loss. When you, as a family member, understand the neurological changes that come with menopause, you’re more likely to notice early signs, encourage healthy habits, and support timely healthcare decisions.
Menopause also sparks important conversations. Maybe you notice your partner struggling with memory lapses, insomnia, or mood changes. Instead of misunderstanding or frustration, knowledge leads to empathy. You might talk openly about symptoms, explore treatment options together, or adjust family routines to offer more support. These small shifts can make a huge difference in a woman’s wellbeing and in the strength of your relationships.
Ultimately, a society that values women’s health and invests in family support during menopause is more resilient. When men, families, and healthcare providers work together, everyone benefits. You’re not just helping one person—you’re helping build a healthier, more connected community for all.
Changing the Old Script: From Stereotype to Empowerment
For far too long, women’s health—and especially the Menopause Impact on the brain—has been sidelined in both society and medicine. As Dr. Lisa Mosconi points out, “Women are important and women’s health matters…and women’s health has not been taken seriously in society and in medicine for hundreds of years.” (2.40–2.45). If you’ve ever felt like your symptoms were brushed aside or misunderstood, you’re not alone. This historic dismissal is finally being challenged, thanks to new Neuroscience Research and a growing movement for Healthcare Provider Education.
It’s easy to see why old stereotypes persist. For centuries, menopause was simply labeled as a time of decline, often linked to emotional instability or frailty. But research shows this narrative is outdated. Dr. Mosconi’s work is flipping the script: menopause is not just an ending, but a time for adaptation and transformation (2.49–2.54). The brain, in particular, undergoes significant changes—some challenging, but many adaptive. Understanding this shift is crucial for both women and the people who support them.
Why does this matter to you? Because the Menopause Impact extends far beyond hot flashes or night sweats. Symptoms like memory lapses, insomnia, and mood changes often originate in the brain, not just the body. Neuroscience Research now reveals that declining estrogen levels can reshape brain structure and function, affecting everything from cognition to emotional regulation. Yet, for generations, these symptoms were dismissed as “just hormones” or, worse, “all in your head.”
This is where Healthcare Provider Education becomes essential. Too many women still report feeling unheard or misunderstood by their doctors. Studies indicate that comprehensive menopause care requires providers to be trained in the latest science—not outdated stereotypes. Dr. Mosconi’s research is at the cutting edge, using advanced brain imaging to show how menopause truly affects women’s minds. When healthcare professionals are educated, they can offer better support, more accurate diagnoses, and effective interventions.
But the responsibility doesn’t stop with doctors. Society as a whole stands to gain from embracing this new understanding. As Dr. Mosconi emphasizes, this isn’t just a “women’s issue”—it’s a societal one (2.59–3.04). Menopause affects mothers, partners, friends, and colleagues. When you support women through this transition, you’re supporting families, workplaces, and communities. Better care leads to more innovative science, improved quality of life, and, ultimately, a healthier society.
- Challenge outdated ideas about menopause and emotional instability.
- Promote accurate knowledge about the neurological changes during menopause.
- Prioritize brain health as a central part of Women’s Health.
Research, not stereotypes, should drive conversations about menopause. The days of minimizing women’s experiences are ending, replaced by data-driven science and a renewed focus on empowerment. A world that takes menopause seriously is a world where women—and their brains—can truly thrive.
Wild Card: If The Brain Was a House—A Quirky Analogy for Menopause
Imagine your brain as a house you’ve lived in for decades. It’s familiar, comfortable, and you know exactly where everything is. Then, menopause arrives—not as a gentle guest, but as a full-scale renovation crew. This isn’t just a minor paint job; it’s new wiring, updated plumbing, and yes, plenty of dust and noise. In the world of cognitive effects, menopause is the ultimate home makeover, reshaping how your mind works and feels.
During the different menopause stages—premenopause, perimenopause, and postmenopause—your brain undergoes a series of changes that can feel disruptive. Think of it like certain rooms being temporarily ‘off-limits’ while the work is underway. For example, the memory room might be cluttered with boxes (hello, brain fog), and the sleep suite could be under noisy construction (cue insomnia and night sweats). But here’s the reassuring part: the foundation of your house—your core self and resilience—remains solid, even when some spaces feel chaotic.
Research shows that these cognitive effects aren’t just random annoyances. Dr. Lisa Mosconi’s groundbreaking brain imaging studies reveal that menopause triggers a significant drop in brain energy—about 30%—as estrogen levels fall. Neurons suddenly can’t burn glucose as efficiently, leading to symptoms like memory lapses and mental fatigue. It’s as if the electrical system in your house is being rewired, causing flickering lights and the occasional power outage. Yet, this process is not about loss alone. It’s about adaptation, reorganization, and the brain’s remarkable ability to rebuild itself for a new stage of life.
How you furnish your newly renovated brain-house matters. Lifestyle adjustments—your choice of diet, exercise, and relationships—are like picking out new furniture, paint colors, and lighting. A Mediterranean-style diet, rich in legumes and fatty fish, acts like high-quality materials that support long-term stability. Regular exercise, especially cardiovascular activities, helps keep the air flowing and the rooms bright. Mind-body practices such as yoga or Pilates can be thought of as cozy rugs and soft lighting, reducing stress and making the space more inviting. Studies indicate that women who make these lifestyle adjustments experience fewer and less severe menopause symptoms, including cognitive effects like brain fog and mood swings.
It’s important to recognize that your choices during and after the renovation shape your comfort and well-being. Personal decisions—what you eat, how you move, the support systems you build—directly influence how your ‘post-construction’ brain feels and functions. Even if some rooms are still under repair, you have the power to create a space that feels safe, functional, and uniquely yours.
Menopause isn’t just a period of loss; it’s a chance for reorganization and growth. Like any major home overhaul, it can be messy and unpredictable, but it also opens up new possibilities. By understanding the cognitive effects and embracing smart lifestyle adjustments, you can turn this renovation into an opportunity to create a brain-house that supports you for years to come.
Frequently Asked Questions: The Menopause & Brain Fog Edition
Menopause is often misunderstood as just a reproductive milestone, but research led by Dr. Lisa Mosconi has shown that it’s a profound neurological event. Many women have questions about what’s happening to their minds during this transition. Here, you’ll find clear, evidence-based answers to the most common queries about menopause symptoms, brain fog, and estrogen decline—helping you navigate this midlife brain makeover with confidence.
What’s the difference between brain fog and early dementia?
It’s natural to worry when you experience memory lapses or trouble focusing during menopause. However, brain fog is a common, temporary symptom linked to estrogen decline and changes in brain energy. Unlike dementia, which involves progressive and severe memory loss that disrupts daily life, menopause-related brain fog usually improves over time. Studies show that up to 62% of women report these cognitive symptoms, but most regain their mental sharpness as their bodies adjust postmenopause. If you notice rapid or worsening memory issues, consult a healthcare provider for a thorough evaluation.
Do all women go through neurological changes in menopause?
Yes, every woman experiences some degree of neurological change during menopause. Dr. Mosconi’s brain imaging research reveals that the drop in estradiol (a key estrogen) triggers a measurable decrease in brain energy, reduced connectivity, and even visible changes in brain structure. Symptoms like hot flashes, insomnia, mood swings, and brain fog are all rooted in these brain changes. However, the severity and type of symptoms can vary widely—factors like genetics, ethnicity, and lifestyle all play a role.
Which foods can really help my brain during menopause?
Diet is a powerful tool for supporting brain health during menopause. Research recommends a Mediterranean-style diet rich in legumes, fatty fish, leafy greens, and healthy fats. These foods provide omega-3 fatty acids and antioxidants, which help reduce inflammation and support cognitive function. Avoiding processed foods, excess sugar, and alcohol is also key, as these can worsen menopause symptoms and brain fog. Staying hydrated and limiting caffeine can further protect your mind and improve sleep quality.
Is hormone therapy always necessary?
Hormone therapy (HRT) isn’t a one-size-fits-all solution. It can be highly effective for some women, especially if started within ten years of the final menstrual period, but it’s not always needed. Newer, lower-dose, and bioidentical hormone options are safer, but lifestyle changes—like exercise, diet, and stress management—can also make a big difference. Always discuss your symptoms and risks with a certified menopause specialist before starting or stopping HRT.
How can symptoms be tracked at home?
Keeping a symptom diary or using digital tracking tools can help you and your healthcare provider spot patterns and triggers. Tools like the Menopause Rating Scale offer a structured way to measure symptom frequency and severity. Research shows that tracking symptoms can help reduce hot flashes and improve quality of life by making it easier to tailor your management plan.
Why should men and families care—and how can they help?
Menopause doesn’t just affect women—it impacts families and communities. When men and loved ones understand menopause symptoms and brain fog, they can offer better support, reduce stigma, and help create a more open environment for discussion. Simple acts like listening, helping with daily tasks, or encouraging healthy habits can make a world of difference.
Can brain health be protected even before menopause begins?
Absolutely. Building brain resilience starts early. Regular exercise, a balanced diet, stress reduction, and avoiding toxins all help maintain healthy brain function and may ease menopause symptoms when the time comes. If you have a family history of early menopause or cognitive decline, these steps are even more important.
Menopause is a major life transition, but it’s also a chance to prioritize your brain health for decades to come. By understanding the science behind menopause symptoms and brain fog, you can take practical steps to protect your mind and well-being—now and in the future.
TL;DR: Menopause doesn’t just change hormones—it rewires the brain. Dr. Lisa Mosconi’s research reveals how symptoms like brain fog and memory lapses are deeply neurological, not just ‘in your head.’ By understanding these changes, using symptom tracking tools, and tweaking your lifestyle, you can take charge of your brain health and thrive through menopause.
A big shoutout to The Diary Of A CEO for their enlightening content! Take a look here: https://youtu.be/Cgo2mD4Pc54?si=AKAI9l-hVsC_6Drh.


Post a Comment